Dr Julinda Lee Jan 18, 2019
Cervical Cancer (HPV) Vaccination

Cervical Cancer and HPV
Cervical cancer is the 4th most common cancer in women. Almost all cases of cervical cancer are related to a persistent infection with the human papillomavirus (HPV). There are more than 150 different types of HPV, with about 13 types known to cause cervical cancer. These types of HPV are also known as “high-risk HPV”.
The types of high-risk HPV most commonly associated with cervical cancer are types 16 and 18, which account for about 70% of all cases of cervical cancer. The rest of cervical cancer are caused by HPV types 31, 33, 45, 52, 58 and a few others.
Besides cervical cancer, HPV can also cause warts around the genital and anal region, and these can be emotionally distressing and difficult to treat even though they are not typically life-threatening. HPV types 6 and 11 account for about 90% of anogenital warts.
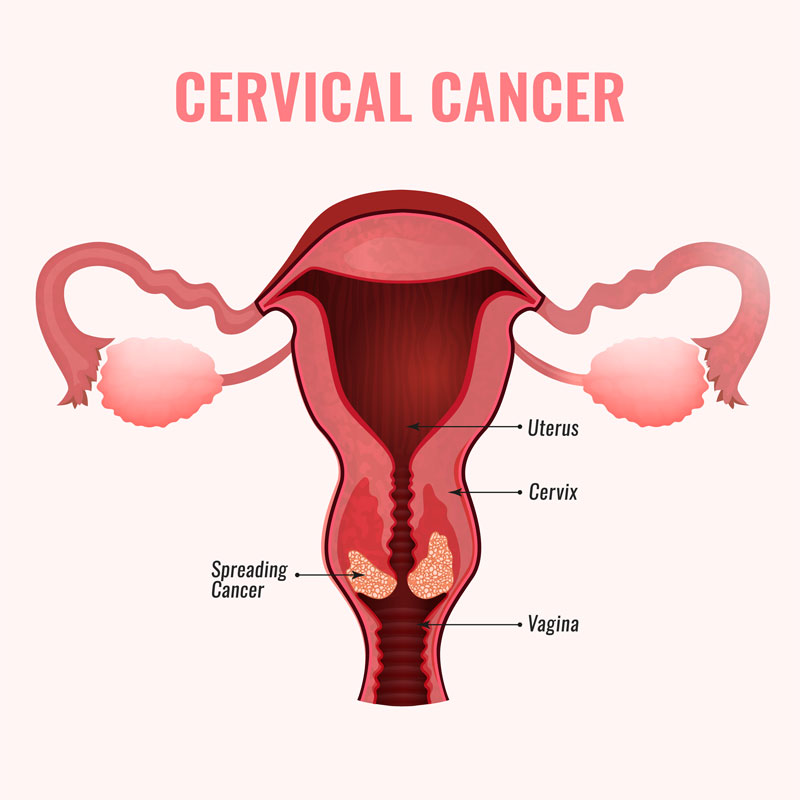
Preventing Cervical Cancer
Since cervical cancer is caused by a virus, preventing an infection by the virus in the first place can prevent cervical cancer. Although it is true that many patients infected with HPV go on to get rid of the infection, there are patients whose immune systems are not able to rid themselves of HPV, which can develop into a pre-cancerous or cancerous change of the cervix.
How HPV Vaccination Works
A vaccine contains the outer coat of the virus (also known as the envelope), and not the live virus and hence cannot result in an infection. The proteins in the envelope of the virus are unique to each strain of HPV. They can induce an immune response when introduced into the body, and result in the production of antibodies by our body’s immune cells. These antibodies heighten our immune response on when we exposed to HPV subsequently, which helps to kill the virus before it can infect our cells.
Your Options for HPV Vaccines
There are different types of vaccines available:
- Cervarix: protects against infection from HPV 16 and 18
- Gardasil 4-valent: protects against infection from HPV 16, 18, 6 and 11
- Gardasil 9-valent: protects against infection from HPV 16, 18, 31, 33, 45, 52, 58, 6 and 11
All HPV vaccines are given in 3 doses, at 0, 2 and 6 months. Since the injection of the vaccine induces an immune response, it is common to have some swelling and pain at the site of the injection. Serious side effects are not common, but you should discuss this in detail with your physician if you have any other medical conditions, as this can affect your response to the vaccine.
Common FAQs
The protection against HPV-related cervical cancer is not 100%, although it is close to 96% with the 9-valent vaccine. Hence, it is still necessary for those who have received the vaccine to undergo screening with Pap smears.
HPV vaccination does not protect against other types of sexually transmitted diseases(STDs) such as herpes simplex virus and HIV, so appropriate use of barrier contraception is also important.
In addition to cervical, vulval and vaginal cancer seen in women, HPV infections are also responsible for a significant proportion of other cancers such as penile cancers and anal cancers. Men who have sex with other men, are more prone to developing anal cancers. In men who have compromised immune systems such as those with a HIV infection, HPV infection is associated with a greater risk of anal cancers.
It is becoming clear that HPV is responsible for other cancers not related to the reproductive tract. While it may be possible to prevent HPV infections during sexual intercourse with the use of condoms, it may be more difficult to prevent HPV infections from oral contact such as through kissing or oral sex. A significant proportion of oropharyngeal and mouth cancers are found to be related to infection with HPV 16, 18 and 33. Vaccinations may potentially prevent against some of these cancers in the head and neck area.
The recommendation that the HPV vaccine should be taken between age 9 and 26 years, is based on the fact that the vaccine was trialed in females in this age group. Ideally, the vaccination should be given prior to any sexual contact, as this will provide the greatest degree of protection. So an older person who has not been exposed to sexual contact, could still consider the vaccination prior to becoming sexually active, and still achieve the same degree of protection.